- Home
- The Mind
- Issue 2023/1
- Issue 2023/2
- Issue 2023/3
- Issue 2024/1
- Issue 2024/2
- Issue 2024/3
- Editorial
- Commentary
- Abstract 1
- Abstract 2
- Abstract 3
- Abstract 4
- Abstract 5
- Abstract 6
- Abstract 7
- Abstract 8
- Abstract 9
- Abstract 10
- Abstract 11
- Abstract 12
- Abstract 13
- Abstract 14
- Abstract 15
- Abstract 16
- Abstract 17
- Abstract 18
- Abstract 19
- Abstract 20
- Abstract 21
- Abstract 22
- Abstract 23
- Abstract 24
- Abstract 25
- Abstract 26
- Abstract 27
- Abstract 28
- Issue 2025/1
- Issue 2025/2
- Contact
- MBMRC
- Events
Opinion
Medicine at the Crossroads of Artificial Intelligence and Human Judgment
by George B. Stefano 1, 2, 3
1Department of Psychiatry, First Faculty of Medicine, Charles University and General University Hospital in Prague, Ke Karlovu 11, 120 00 Prague, Czech Republic
2Distinguished Teaching Prof. Emeritus, Distinguished Academy, State University of New York, USA
3Co-Founder & Co-Chair, Mind-Body Medicine Research Council (MBMRC), Witten/Herdecke University, School of Medicine, Witten, Germany
Cite as: Stefano, G. B. (2025). Medicine at the Crossroads of Artificial Intelligence and Human Judgment. THE MIND Bulletin on Mind-Body Medicine Research, 9(3), X. X
Abstract
The infusion of artificial intelligence (AI), supercomputing, and quantum computing into the field of medicine has accelerated the speed of diagnostic accuracy and therapeutic development. Companies like IBM, Apple, and Google are putting biosensing and analytic technologies into mass-market devices such that health data is democratized and delivered through channels bypassing the old medical gatekeeping. This development creates both opportunity and disruption: biosensor-pushed self-surveillance promotes earlier detection and individually adapted intervention, but can also undermine the old physician’s authority and violate privacy with the harvesting of corporatized data. Telemedicine and the power of AI merge within the hybrid ecosystems of the new clinics, such that the role of the physician must be transformed from sole diagnostician to the unifying interpreter of algorithmic findings. Pre-serving trust and professional integrity within this changing landscape will depend on transparent data stewardship, mutual decision-making, and regulation that ensures the human judgment remains the axis of medical attention
Keywords: Telemedicine, Artificial Intelligence, Augmented Intelligence, super- & Quantum Computing, Biosensors, health care, commercial medicine
The Evolving Role of Computing and AI in Medicine
Supercomputing and quantum computing advances have converted medicine from many reactive fields to predictive and precision medicines (Stefano, 2024; Stefano & Kream, 2017). Technologies like IBM Watson Health exemplify how deep-learning models can assimilate genomic, clinical data with behavioral data to improve diagnosis and treatment suggestions beyond human cognitive potential (Obermeyer & Emanuel, 2016; Rajkomar et al., 2019). Quantum computing extends this potential by simulation of the probabilistic biology of protein folding and neuronal impulses at an unattainable classical computational scale (Biamonte et al., 2017; Stefano, 2024). These developments exemplify what Stefano and Kream (2015, 2023) refer to as the transition to the era of “One Medicine,” in which human and technological fields of knowledge are harmonized under the unifying framework of bioinformatics into the continuum of therapy.
Biosensors and the Consumerization of Medical Insight
The mass commercialization of biosensors—miniaturized devices that can monitor physiological parameters in real time—has placed in the hands of the consumer clinical-grade diagnostics (Stefano & Fernandez, 2017). The Apple Watch and Fitbit now track heart-rhythm irregularities, oxygen saturation levels, and even biomarkers for stress with the aid of AI algorithms (Heikenfeld et al., 2018; Topol, 2015). Although this democratization of data places the power in the hands of the people to be in charge of their own bodily commodity, it also bypasses the physician’s role of interpretation and creates a new interface in which the industry comes between the patient and the professional ( healthcare professional), with such developments signifying the new paradigm in which the health data moves directly from the person to the cloud and not directly from the patient to the doctor (Price & Cohen, 2019; Schwab, 2022).
Telemedicine and the Transformation of Clinical Practice
Telemedicine, spurred on by 5G networks and the integration of AI, illustrates how technologies can re inserts the physician back into the informational loop (Stefano, 2017; Stefano & Kream, 2018). Remote robotic procedures and micro-hospital infrastructure illustrate how digital connectivity can expand the reach of rather than supplant medical expertise (Mehta et al., 2021). Here, biosensor data streams could allow doctors to offer real-time interpretation and intervention, translating raw data into clinical action. This ideal nonetheless hinges on clinicians holding interpretive authority over the insights provided by AI—a dynamic that necessitates new skills in digital literacy, data science, and moral discernment (Topol, 2019; Coiera, 2019).
The Expanding Commerce and the Problem of Professional Degradation
Fears that commercialized AI systems will infiltrate the medical domain are justified. Technology corporations, motivated by the prospect of gain and the acquisition of data assets, may favor algorithmic fine-tuning rather than comprehensive care (Froomkin et al., 2019; Parikh et al., 2019). This process has the potential to sideline clinical judgment and reframe health as a product commodity. The threat is neither the potential of AI but the unmediated commercial brokerdom that exchange professional competence for technological assurance. Stefano (2023) cautions that the entry of AI in the area of diagnostic and neurodegenerative research must be grounded within humancentric oversight and the ethics of medicine. Should clinicians become passive off-takers of machine output, the epistemological basis of the human science of caring known as medicine could be compromised (Cascella et al., 2023; Marcus & Davis, 2020).
Towards Human–Machine Symbiosis in Medicine
The best trajectory is in augmentation of intelligence rather than automation. Following the suggestion of Stefano and Kream (2017), we can consider the potential role of AI to act as an extension of human seeing, similar to molecular mimicry in biology—where functional similarity facilitates complementary rather than replaceable interaction. By the same token in medical care, biosensors and AI must enlarge the cognitive reach of doctors without taking away their interpretive power. Quantum computing's probabilistic simulation and biosensors' real-time sensing create the new epistemic substrate upon which clinical reasoning can be updated dynamically and in the personalized mode (Stefano, 2024; Biamonte et al., 2017). That this development remains ethically framed will be ensured by multidisciplinary regulation involving the combination of computer science, medicine, and philosophy of mind (Floridi & Cowls, 2019; Topol, 2023).
Conclusion and Future Outlook
The introduction of commercialized AI platforms and biosensors into health care is a double-bladed evolution. Whilst it promises new levels of personalization and availability, it also threatens to commodify health and dilute professional judgment. The physician of the future must in turn become a hybrid cognitive agent—part clinician, part data scientist—that includes the ability to integrate algorithmic and experiential knowledge (Topol, 2023; Esteva et al., 2019). Whilst Stefano (2024) and colleagues insist that the intersection of AI, quantum computing, and telemedicine must result in the enlightenment rather than diminution of medicine, it must become an ever more integrated, anticipatory, and patient-centered science.
Authorship contribution statement: Single author
Funding: None
Declaration of competing interest: None
Acknowledgments: None
Data availability: Not applicable
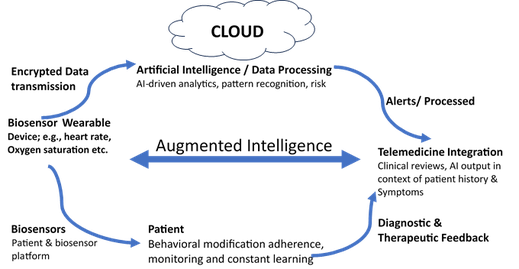
Fig. 1. Conceptual model illustrating the hybrid flow of medical information and decision-making in an augmented intelligence ecosystem. Data originating from biosensors and wearable devices are continuously transmitted to cloud-based artificial intelligence (AI) platforms that perform real-time analysis, pattern recognition, and predictive modeling. These AI-derived outputs are then integrated into telemedicine systems, where physicians interpret results in the context of individual patient histories and physiological trends. Clinical insights and treatment recommendations are communicated back to the patient, completing a continuous feedback loop that enables personalized, dynamic health monitoring. The cyclical architecture underscores the principle of augmented intelligence, in which human expertise, AI computation, and patient participation operate as co-regulatory components of a unified medical ecosystem
References
Biamonte, J., Wittek, P., Pancotti, N., Rebentrost, P., Wiebe, N., and Lloyd, S. (2017). Quantum machine learning. Nature549(7671), 195–202. DOI: 10.1038/nature23474
Cascella, M., Rajnik, M., and Cuomo, A. (2023). Ethical implications of AI in healthcare: A narrative review. Frontiers in Medicine 10, 1179304. DOI: 10.3389/fmed.2023.1179304
Coiera, E. (2019). The forgetting health system. Learning Health Systems 3(3), e10102. DOI: 10.1002/lrh2.10102
Davenport, T., and Kalakota, R. (2019). The potential for artificial intelligence in healthcare. Future Healthcare Journal6(2), 94–98. DOI: 10.7861/futurehosp.6-2-94
Esteva, A., Robicquet, A., Ramos, E., et al. (2019). A guide to deep learning in healthcare. Nature Medicine 25, 24–29. DOI: 10.1038/s41591-018-0316-z
Floridi, L., and Cowls, J. (2019). A unified framework of five principles for AI in society. Harvard Data Science Review1(1). DOI: 10.1162/99608f92.8cd550d1
Froomkin, A. M., Calo, R., and Rao, A. (2019). When AIs outperform doctors: Confronting the challenges of a tort-induced overreliance on machine learning. Arizona Law Review 61(1), 33–99.
Heikenfeld, J., Jajack, A., Rogers, J., Ghaffari, R., Stahl, R., Muck, A., et al. (2018). Wearable sensors: Modalities, challenges, and prospects. Lab on a Chip 18, 217–248. DOI: 10.1039/C7LC00914C
Marcus, G., and Davis, E. (2020). Rebooting AI: Building Artificial Intelligence We Can Trust. Pantheon Books.
Mehta, N., Cali, S., and Appelboom, G. (2021). The role of 5G networks in telemedicine and robotic surgery. Frontiers in Surgery 8, 598955. DOI: 10.3389/fsurg.2021.598955
Obermeyer, Z., and Emanuel, E. J. (2016). Predicting the future—big data, machine learning, and clinical medicine. New England Journal of Medicine 375(13), 1216–1219. DOI: 10.1056/NEJMp1606181
Parikh, R. B., Obermeyer, Z., and Navathe, A. S. (2019). Regulation of predictive analytics in medicine. Science363(6429), 810–812. DOI: 10.1126/science.aaw0029
Price, W. N., and Cohen, I. G. (2019). Privacy in the age of medical big data. Nature Medicine 25(1), 37–43. DOI: 10.1038/s41591-018-0272-7
Rajkomar, A., Dean, J., and Kohane, I. (2019). Machine learning in medicine. New England Journal of Medicine 380, 1347–1359. DOI: 10.1056/NEJMra1814259
Schwab, K. (2022). The Fourth Industrial Revolution: Implications for Healthcare. World Economic Forum Reports.
Stefano, G. B. (2017). Robotic surgery: Fast forward to telemedicine. Medical Science Monitor 23, 1856.
Stefano, G. B. (2023). Artificial intelligence as a tool for the diagnosis and treatment of neurodegenerative diseases. Brain Sciences 13(6), 938.
Stefano, G. B. (2023). Personalized and One Medicine coming together. The Mind, 1–2. DOI: 10.61936/themind/202301311
Stefano, G. B. (2024). Quantum computing and artificial intelligence: Disruptive technology with potential applications in surgical practice. Journal of Surgery 9. DOI: 10.29011/2575-9760.001974
Stefano, G. B. (2024). Quantum computing and the future of neurodegeneration and mental health research. Brain Sciences 14, 93. DOI: 10.3390/brainsci14010093
Stefano, G. B., and Fernandez, E. A. (2017). Biosensors: Enhancing the natural ability to sense and their dependence on bioinformatics. Medical Science Monitor 23, 3168–3169.
Stefano, G. B., and Kream, R. M. (2015). Personalized- and One-Medicine: Bioinformatics foundation in health and its economic feasibility. Medical Science Monitor 21, 201–204.
Stefano, G. B., and Kream, R. M. (2017). Artificial intelligence, DNA mimicry, and human health. Medical Science Monitor 23, 3923–3924.
Stefano, G. B., and Kream, R. M. (2018). The micro-hospital: 5G telemedicine-based care. Medical Science Monitor Basic Research 24, 103–104.
Topol, E. J. (2015). The Patient Will See You Now: The Future of Medicine Is in Your Hands. Basic Books.
Topol, E. J. (2019). High-performance medicine: The convergence of human and artificial intelligence. Nature Medicine25(1), 44–56. DOI: 10.1038/s41591-018-0300-7
Topol, E. J. (2023). Deep Medicine: How Artificial Intelligence Can Make Healthcare Human Again. Hachette UK.