- Home
- The Mind
- Issue 2023/1
- Issue 2023/2
- Issue 2023/3
- Issue 2024/1
- Issue 2024/2
- Issue 2024/3
- Editorial
- Commentary
- Abstract 1
- Abstract 2
- Abstract 3
- Abstract 4
- Abstract 5
- Abstract 6
- Abstract 7
- Abstract 8
- Abstract 9
- Abstract 10
- Abstract 11
- Abstract 12
- Abstract 13
- Abstract 14
- Abstract 15
- Abstract 16
- Abstract 17
- Abstract 18
- Abstract 19
- Abstract 20
- Abstract 21
- Abstract 22
- Abstract 23
- Abstract 24
- Abstract 25
- Abstract 26
- Abstract 27
- Abstract 28
- Issue 2025/1
- Issue 2025/2
- Issue 2025/3
- Contact
- MBMRC
- Events
Report 1
Precision breathing: AI-personalised MBM microinterventions for sleep and stress in adolescence
by Yvonne Beerenbrock1
1Professorship for Quality of Life, Spirituality and Coping, Faculty of Health, Medical Department, Institute of Integrative Medicine, Witten/Herdecke University, Witten, Germany
Cite as: Beerenbrock, Y. (2025). Precision breathing: AI-personalised MBM microinterventions for sleep and stress in adolescence. THE MIND Bulletin on Mind-Body Medicine Research, 9(3), 24-32. https://doi.org/10.61936/themind/202511176
Abstract
With the onset of puberty, the internal clock shifts backwards, creating a structural mismatch with early school hours. This conflict results in reduced sleep duration, daytime fatigue and a decline in mood and performance. Structural reforms such as later start times alleviate the burden, but leave the evening self-control bottleneck intact. This is precisely where low-threshold, immediately effective help is needed. Precision breathing offers such micro-interventions: ultra-short, inconspicuous breathing sequences that young people can use independently during transitions. Because slow, exhalation-focused and resonance-oriented breathing promotes vagal regulation, it reduces arousal and facilitates the transition to sleep readiness. To ensure that the effect is not left to chance, these micro-interventions are designed as Just-in-Time Adaptive Interventions (JITAI): AI personalises the timing, dose and technique to the condition, context and progression. This requires data minimisation, transparency, opt-out options and fairness audits to ensure autonomy and justice. In this way, precision breathing combines structural and subjective logic. The next step is methodologically robust micro-randomised studies with valid measurement and school-based implementation.
Keywords: Adolescence; Precision Breathing; Micro-interventions; Sleep Regulation; Stress Regulation; Just-in-Time Adaptive Interventions (JITAI)
Why Breathing Micro-Interventions in Adolescence?
The circadian rhythm systematically shifts backwards during puberty, leading to a structural discrepancy between biological sleep tendencies and early school hours. This has well documented consequences: less sleep, more tiredness during the day, and a drop in mood and performance (Yip et al., 2022; Minges & Redeker, 2016). Delayed school start times have demonstrated benefits in alleviating these conditions by extending sleep duration and improving well-being (Barlaan et al., 2022; Yip et al., 2022) – however, they are not implemented across the board, nor do they eliminate the second bottleneck of daily life that occurs in the evening: High screen exposure, homework and social-emotional activation increase arousal making it difficult to ‘switch off’ (Crowley et al., 2018). This is consistently associated with poorer sleep in cohort and review studies (Brosnan et al., 2024; Drumheller & Fan, 2022).
Here is where micro-interventions for breathing fill the gap: ultra-short, low-impact exercises lasting three to five minutes that young people can implement independently during transitional phases (after learning phases, before exams, in their evening routine). Young people need easy-to-use and effective self-regulation tools and precision breathing is exactly that. Slow, steady breathing at a rate of approximately 4.5–7 breaths per minute increases respiratory sinus arrhythmia, strengthens baroreflex dynamics and promotes vagal activity (Bentley et al., 2022). These effects have been consistently associated with calmed physical arousal, improved emotional control, and benign cardiovascular modulation (Laborde et al., 2022; Russo et al., 2017).
Exhalation-oriented approaches such as cyclical sighing show significant improvements in affect and reductions in tension after just 5 minutes daily in a randomised study (Balban et al., 2023). Kramer et al. (2023) showed that effectiveness is context-dependent, as breathing exercises are most effective when they are offered just-in-time on moments of anxiety or high stress (Nahum-Shani et al., 2018). At the same time, the individual frequency at which people resonate with such interventions is not rigid but variable, so that maximum benefit is achieved with a personalised target frequency rather than a ‘one-size-fits-all’ approach (Yoo et al., 2022; Lehrer & Gevirtz, 2014). For use before bedtime, polysomnographic pilot data support the use of slow breathing to reduce alertness and promote sleep-inducing states (Kuula et al., 2020). In addition, school-based cluster pilot studies demonstrate feasibility, acceptance, and stress reduction in real-world settings (Bentley et al., 2022). Furthermore, micro-randomised, digitally supported sleep Just-in-Time Adaptive Interventions (JITAIs) show improvements in sleep stability and daytime well-being under field conditions, indicating the feasibility of context-sensitive, micro-dosed sleep interventions (Takeuchi et al., 2024).
Microinterventions as shown in Table 1 for breathing thus combine structural and subjective logic, as they complement the (as-yet unevenly implemented) structural reform of later school start times by offering young people a concrete, immediately effective coping strategy for self-regulation, especially in the evening and during stressful times of the day. In short, educational policy-based prevention can create more opportunities for adequate sleep, while micro-interventions help to make the most of these opportunities.
From breathing exercises to MBM micro-interventions
When there is an acute need for relaxation, sequences focused on exhalation are recommended. In a randomised study, just 5 minutes daily showed a noticeable improvement in mood and reduction in tension (Balban et al., 2023). For periods of rest, such as during longer school breaks, steady, slow breathing stabilises the parasympathetic nervous system. And in the evening routine, 5–10-minute presleep protocols act as a ritualised ‘gateway’ to sleep readiness (Kuula et al., 2020). A three-part administration format is therefore required: (1) rapid effect during peaks of stress, (2) longer-lasting regulation during the day, and (3) to accompany sleep in the evening.
This logic does not end in standardised administration. Young people differ significantly in terms of physiology, temperament, chronotype, fitness level and contexts, and the individual resonance frequency of their breathing also varies. Precision breathing is therefore not a one-size-fits-all solution, but requires a short, learning calibration: Initial breathing pacing (3–5 minutes) with heart rate variability (HRV) feedback determines a personalised target frequency, which can be fine-tuned as the situation requires (e.g. slightly slower in the evening, minimally higher before exams) in order to make optimal use of Respiratory Sinus Arrhythmia (RSA) resonance (Lehrer & Gevirtz, 2014).
Methodological care is required: many wearables estimate HRV photoplethysmographically as pulse rate variability (PRV). PRV is sufficiently meaningful during rest and sleep phases, but not identical to Electrocardiography (ECG) HRV. Decision rules should therefore provide for quality filters, artifact checks and rest reference windows to avoid false triggers and ensure reliability (Kantrowitz et al., 2025).
AI personalisation as JITAI: decision architecture
In order to join structural and subjective logic, young people should acquire self-management skills in the micro-rhythm of everyday life. A Just-in-Time Adaptive Intervention (JITAI) with AI personalisation is an approach that bridges this gap. Its basic principle is simple but difficult to implement: not ‘more intervention’, but the right intervention at the right time is needed. First, the framework defines proximal target variables such as reducing anxiety or somatic tension within a ten-minute time window and alleviating physical and psychological stress reactions before falling asleep. This is followed by decision points as shown in Table 2 based on the daily rhythm of young people (school breaks, before exams, after homework, at the threshold of sleep). Tailored variables record situational stress experiences and contextual conditions such as subjective stress and rumination, time of day and day of the week, sleep history, the last intervention, and simple physiological short markers such as PRV- Root Mean Square of Successive Differences (RMSSD) from wearables. Based on this assessment, the system chooses between different intervention options (exhalation-focused relaxation, resonance breathing or consciously no intervention) according to clear decision rules that avoid overstimulation and respect autonomy (Nahum-Shani et al., 2018; Klasnja et al., 2015).
The learning logic should be adaptive. This is ensured by contextual bandit algorithms that strike a balance between exploration and exploitation. While initially testing cautiously which micro-intervention is effective in which context, the system prefers the option that is expected to provide the greatest immediate benefit for that person under these conditions as evidence increases. Micro-randomised designs provide the causal short-term effect for this, so that the strategy is based on empirical excursion effects rather than intuition. This creates a learning logic in care that does not smooth out heterogeneity but uses it productively (Tewari & Murphy, 2017; Liao et al., 2020; Greenewald et al., 2017). The practical design consists of a lean mix of sensors from passive contexts (time of day, simple calendar events), PRV references recorded at night as a stable baseline, economic digital usage indicators, and ultra-short self-reports (one question about stress or sleepiness).
From the receptivity (availability without distraction) and the necessity (increased stress level, rumination before bedtime), the AI derives tailored suggestions, such as three minutes of exhalation-focused breathing before an exam or five minutes of resonance breathing in the evening routine, embedded in soft constraints (maximum number of prompts per day, fixed rest periods, option to opt out at any time) (Klasnja et al., 2015; Nahum-Shani et al., 2018; Liao et al., 2020). The target architecture remains multi-layered: (1) in the short term, stress reaction, heart rate and respiratory rate decrease; (2) in the medium term, days with short sleep latency increase; (3) in the long term, sleep duration and daytime functioning stabilise, while (4) school stress and anxiety decrease. Engagement is measured objectively (traces of use, mini- Ecological momentary assessments (EMA)) to improve enabling conditions (Leong et al., 2023). In this way, the JITAI decision-making architecture as shown in Figure 1 combines educational connectivity with technical precision and strengthens young people's self-control without overforming their living environment.
Security, Ethics & Fairness
Health promotion requires age-appropriate consent procedures, understandable information routes and a genuine freedom of choice. Young people need to know what data is being collected and for what purpose, and what rights they have, because only then can self-determination become a real option and not just an appeal (Agostino et al., 2023; Mathews, 2022). Technically, this leads to the principle of data minimisation and, where possible, edge processing, so that sensitive data remains on the device and only aggregated/purpose-specific information is processed. An opt-out without disadvantages is essential, as autonomy in adolescence must be structurally guaranteed for educational reasons (Agostino et al., 2023).
Digital prediction models are not neutral, as they easily reflect and reinforce existing inequalities when training data and decision chains contain demographic biases (Obermeyer et al., 2019). For youth-oriented applications, regular algorithm audits and fairness corrections are therefore imperative, e.g. through demographically informed reweighting or procedures to reduce disparate effects (Park et al., 2022; Ueda et al., 2023). The normative standard is that equal opportunities go hand in hand with effective support, regardless of gender, origin, socio-economic status or neurodiversity.
It is equally important that services for young people are developed together with young people. Co-design formats therefore highlight experiential knowledge, increase acceptance and accuracy, and reduce misjudgements based on adult-centred assumptions (Oetken et al., 2024). This includes transparency about the trigger logic (when, why and on what basis is a proposal made?) as well as maintaining the ability to act through inviting, moderate proposals that fit the rhythm of life, avoid disruption and can be rejected at any time (Nahum-Shani et al., 2018).
Author Contributions: Conceptualization, Y.B.; investigation, Y.B.; writing—review and editing, Y.B.; All authors have read and agreed to this version of the manuscript.
Funding: This research received no external funding.
Institutional Review Board Statement: Not applicable.
Informed Consent Statement: Not applicable.
Data Availability Statement: No data was used in this commentary article.
Conflicts of Interest: The authors declare no conflicts of interest.
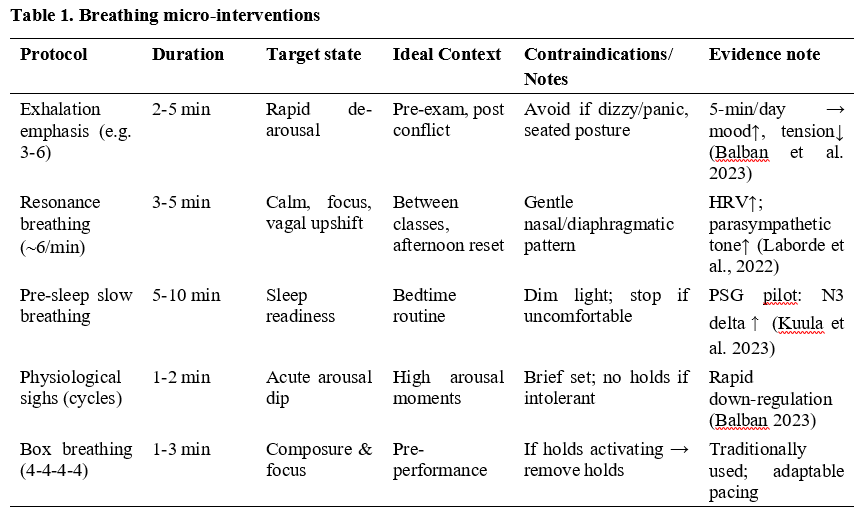


Figure 1. Just-in-time decision architecture for precise breathing in adolescence. The diagram links structural rhythms (school day, evening routines) with subjective self-regulation: Passive and minimal signals (time of day, calendar, nocturnal PRV baseline, ultra-short EMA) determine eligibility as a joint function of need (increased stress or rumination before bedtime) and receptivity (no competing demands). Decision rules operationalise a contextual bandit policy with a ‘non-intervention’ arm and soft constraints (≤3 prompts/day; rest periods) and select a microintervention (exhale 3′, resonance 5′, box 2′) that is discreet and executable with a tap of the finger. A proximal outcome check (Δ stress at 10'; Δ HR/BR at 5'; immediate acceptance) feeds into the policy update (exploration→evaluation; change/adjustment for non-responders).
References
Agostino, H., & Toulany, A. (2023). Considerations for privacy and confidentiality in adolescent health care service delivery. Paediatrics & child health, 28(3), 172–183. https://doi.org/10.1093/pch/pxac117.
Balban, M. Y., Severs, L. J., Naeini, E., et al. (2023). Brief structured respiration practices enhance mood and reduce physiological arousal compared to mindfulness meditation. Cell Reports Medicine, 4(1), 100895. https://doi.org/10.1016/j.xcrm.2022.100895.
Barlaan, D. R., Pangelinan, B. A., Johns, A., Schweikhard, A., & Cromer, L. D. (2022). Middle school start times and young adolescent sleep, behavioral health, and academic performance outcomes: a narrative review. Journal of clinical sleep medicine : JCSM : official publication of the American Academy of Sleep Medicine, 18(11), 2681–2694. https://doi.org/10.5664/jcsm.10224.
Bentley, T. G. K., Seeber, C., Hightower, E., Mackenzie, B., Wilson, R., Velazquez, A., Cheng, A., Arce, N. N., & Lorenz, K. A. (2022). Slow-Breathing Curriculum for Stress Reduction in High School Students: Lessons Learned From a Feasibility Pilot. Frontiers in rehabilitation sciences, 3, 864079. https://doi.org/10.3389/fresc.2022.864079.
Brosnan, B., Haszard, J. J., Meredith-Jones, K. A., Wickham, S. R., Galland, B. C., & Taylor, R. W. (2024). Screen Use at Bedtime and Sleep Duration and Quality Among Youths. JAMA pediatrics, 178(11), 1147–1154. https://doi.org/10.1001/jamapediatrics.2024.2914.
Crowley, S. J., Wolfson, A. R., Tarokh, L., & Carskadon, M. A. (2018). An update on adolescent sleep: New evidence informing the perfect storm model. Current Opinion in Psychology, 8, 50–56. https://doi.org/10.1016/j.copsyc.2018.02.021.
Doherty, C., Baldwin, M., Keogh, A., Caulfield, B., & Argent, R. (2024). Keepingjust with Wearables: A Living Umbrella Review of Systematic Reviews Evaluating the Accuracy of Consumer Wearable Technologies in Health Measurement. Sports medicine (Auckland, N.Z.), 54(11), 2907–2926. https://doi.org/10.1007/s40279-024-02077-2.
Drumheller, K., & Fan, C. W. (2022). Unprecedented times and uncertain connections: A systematic review examining sleep problems and screentime during the COVID-19 pandemic. Sleep epidemiology, 2, 100029. https://doi.org/10.1016/j.sleepe.2022.100029.
Easton, S., Ainsworth, B., Thomas, M., Latter, S., Knibb, R., Cook, A., Wilding, S., Bahrami-Hessari, M., Kennington, E., Gibson, D., Wilkins, H., Yardley, L., & Roberts, G. (2022). Planning a digital intervention for adolescents with asthma (BREATHE4T): A theory-, evidence- and Person-Based Approach to identify key behavioural issues. Pediatric pulmonology, 57(11), 2589–2602. https://doi.org/10.1002/ppul.26099.
Greenewald, K., Tewari, A., Klasnja, P., & Murphy, S. (2017). Action Centered Contextual Bandits. Advances in neural information processing systems, 30, 5973–5981. https://doi.org/10.48550/arXiv.1711.03596
Kantrowitz, A. B., Ben-David, K., Morris, M., Wittels, H. L., Wishon, M. J., McDonald, S. M., Renaghan, E. J., Feigenbaum, L. A., & Wittels, S. H. (2025). Pulse rate variability is not the same as heart rate variability: findings from a large, diverse clinical population study. Frontiers in physiology, 16, 1630032. https://doi.org/10.3389/fphys.2025.1630032.
Klasnja, P., Hekler, E. B., Shiffman, S., Boruvka, A., Almirall, D., Tewari, A., & Murphy, S. A. (2015). Microrandomized trials: An experimental design for developing just-in-time adaptive interventions. Health psychology : official journal of the Division of Health Psychology, American Psychological Association, 34S(0), 1220–1228. https://doi.org/10.1037/hea0000305.
Kramer, A. C., Neubauer, A. B., & Schmiedek, F. (2023). The Effectiveness of A Slow-Paced Diaphragmatic Breathing Exercise in Children's Daily Life: A Micro-Randomized Trial. Journal of clinical child and adolescent psychology : the official journal for the Society of Clinical Child and Adolescent Psychology, American Psychological Association, Division 53, 52(6), 797–810. https://doi.org/10.1080/15374416.2022.2084743.
Kuula, L., Halonen, R., Kajanto, K., Lipsanen, J., Makkonen, T., Peltonen, M., & Pesonen, A. K. (2020). The Effects of Presleep Slow Breathing and Music Listening on Polysomnographic Sleep Measures - a pilot trial. Scientific reports, 10(1), 7427. https://doi.org/10.1038/s41598-020-64218-7.
Laborde, S., Allen, M. S., Borges, U., Dosseville, F., Hosang, T. J., Iskra, M., Mosley, E., Salvotti, C., Spolverato, L., Zammit, N., & Javelle, F. (2022). Effects of voluntary slow breathing on heart rate and heart rate variability: A systematic review and a meta-analysis. Neuroscience and biobehavioral reviews, 138, 104711. https://doi.org/10.1016/j.neubiorev.2022.104711.
Lehrer, P. M., & Gevirtz, R. (2014). Heart rate variability biofeedback: how and why does it work?. Frontiers in psychology, 5, 756. https://doi.org/10.3389/fpsyg.2014.00756.
Leong, U., & Chakraborty, B. (2023). Participant Engagement in Microrandomized Trials of mHealth Interventions: Scoping Review. JMIR mHealth and uHealth, 11, e44685. https://doi.org/10.2196/44685.
Mathews, B. (2023). Adolescent Capacity to Consent to Participate in Research: A Review and Analysis Informed by Law, Human Rights, Ethics, and Developmental Science. Laws, 12(1), 2. https://doi.org/10.3390/laws12010002.
Minges, K. E., & Redeker, N. S. (2016). Delayed school start times and adolescent sleep: A systematic review of the experimental evidence. Sleep Medicine Reviews, 28, 86–95. https://doi.org/10.1016/j.smrv.2015.06.002.
Nahum‑Shani, I., Smith, S. N., Spring, B. J., Collins, L. M., Witkiewitz, K., Tewari, A., & Murphy, S. A. (2018). Just‑in‑time adaptive interventions in mobile health: Key components and design principles. Annals of Behavioral Medicine, 52(6), 446–462. https://doi.org/10.1007/s12160-016-9830-8.
Obermeyer, Z., Powers, B., Vogeli, C., & Mullainathan, S. (2019). Dissecting racial bias in an algorithm used to manage the health of populations. Science (New York, N.Y.), 366(6464), 447–453. https://doi.org/10.1126/science.aax2342.
Oetken, K. J., Hennig, K., Henkel, S., & Merfeld, K. (2024). A psychoanalytical approach in urban design: exploring dynamics of co-creation through theme-centred interaction. Journal of Urban Design, 30(4), 445–472. https://doi.org/10.1080/13574809.2024.2351911.
Park, J., Arunachalam, R., Silenzio, V., & Singh, V. K. (2022). Fairness in Mobile Phone-Based Mental Health Assessment Algorithms: Exploratory Study. JMIR formative research, 6(6), e34366. https://doi.org/10.2196/34366.
Russo, M. A., Santarelli, D. M., & O'Rourke, D. (2017). The physiological effects of slow breathing in the healthy human. Breathe (Sheffield, England), 13(4), 298–309. https://doi.org/10.1183/20734735.009817.
Takeuchi, H., Ishizawa, T., Kishi, A., Nakamura, T., Yoshiuchi, K., & Yamamoto, Y. (2024). Just-in-Time Adaptive Intervention for Stabilizing Sleep Hours of Japanese Workers: Microrandomized Trial. Journal of medical Internet research, 26, e49669. https://doi.org/10.2196/49669.
Tewari, A., Murphy, S.A. (2017). From Ads to Interventions: Contextual Bandits in Mobile Health. In: Rehg, J., Murphy, S., Kumar, S. (eds) Mobile Health. Springer, Cham. https://doi.org/10.1007/978-3-319-51394-2_25.
Tsakona, P., Kitsatis, I., Apostolou, T., Papadopoulou, O., & Hristara-Papadopoulou, A. (2025). The Effect of Diaphragmatic Breathing as a Complementary Therapeutic Strategy in Stress of Children and Teenagers 6-18 Years Old. Children (Basel, Switzerland), 12(1), 59. https://doi.org/10.3390/children12010059.
Ueda, D., Kakinuma, T., Fujita, S., Kamagata, K., Fushimi, Y., Ito, R., Matsui, Y., Nozaki, T., Nakaura, T., Fujima, N., Tatsugami, F., Yanagawa, M., Hirata, K., Yamada, A., Tsuboyama, T., Kawamura, M., Fujioka, T., & Naganawa, S. (2024). Fairness of artificial intelligence in healthcare: review and recommendations. Japanese journal of radiology, 42(1), 3–15. https://doi.org/10.1007/s11604-023-01474-3.
Wheaton, A. G., Chapman, D. P., & Croft, J. B. (2016). School Start Times, Sleep, Behavioral, Health, and Academic Outcomes: A Review of the Literature. The Journal of school health, 86(5), 363–381. https://doi.org/10.1111/josh.12388.
Yip, T., Wang, Y., Xie, M., Ip, P. S., Fowle, J., & Buckhalt, J. (2022). School Start Times, Sleep, and Youth Outcomes: A Meta-analysis. Pediatrics, 149(6), e2021054068. https://doi.org/10.1542/peds.2021-054068.
Yoo, H. J., Nashiro, K., Min, J., Cho, C., Bachman, S. L., Nasseri, P., Porat, S., Dutt, S., Grigoryan, V., Choi, P., Thayer, J. F., Lehrer, P. M., Chang, C., & Mather, M. (2022). Heart rate variability (HRV) changes and cortical volume changes in a randomized trial of five weeks of daily HRV biofeedback in younger and older adults. International journal of psychophysiology : Official journal of the International Organization of Psychophysiology, 181, 50–63. https://doi.org/10.1016/j.ijpsycho.2022.08.006.